November 14th, 2016. 20:10.
This is not happening. Numbness. Time stood still as we stared blankly ahead watching the chaos unfold in front of us.
That morning was different than any other that we’d experienced because we knew that something was different – we would be leaving our home of 2 months. Logically, we knew it was a good thing but leaving was hard – the people in the PCICU were family and frankly, they were more qualified to look after Laura than anyone else!
Our transition meeting was supposed to happen at 10:00 so we got to the unit around 07:00 to ensure we had plenty of time for cuddles and stories before the meeting. Due to some scheduling problems with different members of the team, the meeting got pushed to 14:30 – no big deal, more time to hang out with Laura.
This morning I held Laura against my chest. This seems like a normal thing but for a mom of a kid that’s been intubated/on CPAP, etc for most of their life, it is a big deal.
Being able to hold Laura any way I chose was a pretty exciting thing! Before we headed for the meeting Laura had her usual daily ECG and blood work and then we got to play and hold her for the rest of the morning and early afternoon.
At 14:30, one of the social workers came to get us to bring us to the meeting – she would be there to be sure all of our concerns were heard and addressed.
The meeting was not that exciting – it consisted of members of the PCICU team and members of the team on 4C, the “floors” where the cardiac kids went when they were well on the road to recovery. Lindsay laid out the gist of Laura’s history and then spent about twice that much time pleading with the team to take their time with everything they do – Laura is unpredictable. Thanks Lindsay… it was true of course but still – Laura’s better now! Also at the meeting was Dr. Simon who explained some of the plan for the treatment of Laura’s failing left ventricle and T. (I’ll use her initial because I haven’t received permission to use her real name yet) – the respiratory therapist who just that day had taken on the role of overseeing the care of all cardiac children. She also happened to be one of Laura’s ECMO specialists and we love her dearly – she is hilarious and blunt (I can appreciate that). She helped to lay out the complicated history Laura already had with her ventilatory support.
We also discussed when we would be returning to Saskatoon – the decision was that we would spend a week or two upstairs and if all went well, we would discuss a transfer (it was insane to think that we could be in our own province soon!).
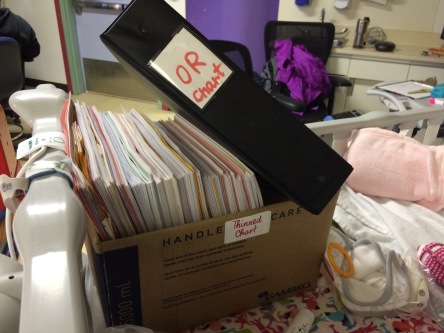
After the meeting we headed back to the unit to be with Laura and wait for the transfer. At 16:00 we received the go ahead and we packed up all of Laura’s things (including her chart which was the normal binder followed by a couple boxes) and headed upstairs.
Laura apparently missed her friends already because she made her presence known in the hallways as she screamed until she was beet red the whole way.
Once settled in the ICE room (Intermediate Care Environment) and handover was finished, we met the nurse that would be caring for Laura and discussed her history a bit. The nurse was very kind and helped us to feel comfortable in our new home. It was nice to be able to have a little more freedom in taking care of Laura – we were shown where to get all of the supplies and toys ourselves rather than having to pester the nurse like we would in the PCICU – maybe this wouldn’t be so bad.

A little while after we arrived, one of the cardiac fellows that we had already met a few times came to chat with us. She told us that on Laura’s ECG her ST elevation was slightly more pronounced (Laura had pretty bad ST elevation for a couple weeks now but it had not been affecting her clinically or on her echos so we chose to ignore it). Because of this they ran a troponin test with her regular daily bloodwork – it had come back as slighly elevated. Troponin is a hormone that the body secretes that let’s you know that something is going wrong with the heart – in an adult it is a marker for a heart attack but in a child it is slightly less clear cut. We were going to keep an eye on her levels over the night shift but with her clinical status and latest echo being good – we weren’t too concerned. She explained that it is the whole picture that matters – we can’t focus on one bad test.
My heart sunk and I felt a pit in my stomach but I pushed it away because I trusted the team and if they aren’t worried – I shouldn’t be either.
We went to get some supper and ate quickly while Laura napped so that we could come back to see her. We sat by her bedside and tried to decide when we’d be heading home that night – maybe we’d stop at Wal Mart and buy her something for making the trip upstairs.
At 19:00, the new shift started and we met Laura’s nurse for the evening. His first words to us were “she’s coded before right?” – I felt like this was not an overly kind first impression but I suppose if I were her nurse I’d want to know that information too. He then let us know that he’d be drawing her troponin level again at 20:00 and then again at 04:00 so that we could see if her level was rising or returning to normal.
At 20:00 the RT came by to change Laura from highflow to CPAP and I stood on the other side of her bed to help him with her tapes. Laura had some fancy tape work that had been perfected down in the PCICU to help protect her sensitive skin from the mask so that she wouldn’t permanently look like she had just been beat up. Before we started the nurse drew the troponin level and then went to care for another patient.
20:10 – A.J. noticed Laura’s heart rate looking a little funny and it dropped from 140ish (she was mad because we were changing her tapes – she usually sat at 120) to 110. I looked up at the monitor and it continued to go down – 107, 104 – I thought maybe her leads had come off so I ripped open the buttons on her sleeper to have a look.
In an instant, Laura’s heart rate plummeted and as I was standing there looking at the leads her chest changed from pink to grey. The immediacy in which her colour changed was astounding – she no longer looked alive – she stopped crying, went limp and lost all life and colour. I quickly turned towards the window to the nurses desk and said
It’s real.
By the time I had begun uttering the words, Laura’s nurse was right there taking my place as I gladly stepped back and he began compressions. He called for help and another nurse came and ripped the emergency line out of the wall to set off the alarm. A.J and I stepped back from the foot of Laura’s bed – far enough that we weren’t in the way but close enough to see what was happening. In a matter of seconds a swarm of nurses showed up. The RT that had been changing her tapes had already begun bagging Laura to give her the oxygen she needed and another nurse placed the board under Laura’s lifeless body to allow the compressions to go deeper into her chest.
This is not happening. Numbness. Time stood still as we stared blankly ahead watching the chaos unfold in front of us.
I wasn’t thinking or feeling – I was just standing, trembling, clinging onto A.J’s hand and watching- how lucky am I to have that kind of a support standing right there?
The code was run like a beautiful ballet in slow motion.
The baby coded. A nurse began compressions. The alarm sounded.
Instantly a large group showed up to help. They formed a line so that no one person is doing compressions for longer than they can handle. One nurse began charting while another took the role of calling out times and events to record. The code team was called. The crash cart arrived.
Where are they?
They were the only words I could think of and they were the first and only words I said to A.J during the code. The pit in my stomach grew deeper with every second that I didn’t see one of our doctors – our family. Why weren’t they here yet? How long would it take for them to run up the stairs and get to us? These people were doing their job but it’s not the same – we need the experts.
Shortly after I uttered the words an angel appeared – Paula. The sheer sight of her sent a wave of calm over my body and I felt myself grow just a little bit less tense. She was here – she would fix this. Until she showed up my mind was full of questions – how do I tell our family? What do I do with the nursery? How do I live without her?
But as soon as I saw Paula’s face – my mind switched – Will she need ECMO? Does this mean we need a transplant? Do you see the difference in these questions? These questions assume that Laura would come back to us.
She immediately sprung into action:
Push harder. Faster. Where is the epi? I need it now.
She began clapping out the pace at which the compressions needed to happen – she was not letting Laura’s brain go any longer with insufficient oxygen.
Moments after taking charge, Dominic showed up. He was the doctor on the code team for the week so Paula stepped back and handed the reigns over to him. She came over to us and put her arm around us – this is when the tears began. Until this moment, I felt as if my body and mind were separate but that touch brought me back together. She told us that she was on anesthesia for the week and had been heading home when she heard the code and came running – hoping and praying that it wasn’t Laura again.
Dominic took charge and gave Laura a large dose of epi into her picc line. Within seconds, she began crying. Many people say that the sound of a newborn crying after birth is the best sound – that’s not true – this cry was the best sound I had ever heard. Compressions stopped, the time was called out, and Dominic left the RT to get her cpap back on at 100% oxygen while the nurses began getting her ready to be taken back down to the PCICU. She regained much of her colour instantly and began moving around again. She was mad – good. She should be mad.
Dominic came over to talk to us. All he could think of was “I’m so sorry.” I asked him the question of the hour:
Did she look AT you?
This question seems silly but we had been around the block enough to know that even though Laura was pink and breathing, that did not mean that she was still there. Her brain had suffered a second cardiac arrest – this is a lot for a little body to handle. Dominic replied, ever so eloquently, like always in his British accent:
She looked up AT me and was pissed off AT me.
Laura and Dominic had always had an interesting relationship – he had been her anesthesiologist countless times but she never really liked him. When he would talk she would cry – so this meant more than just anyone saying that she was mad at them.
They prepared Laura for transport and Dominic went with her while we gathered her things – we had unpacked into the cubbies that they had provided. While we packed, Simon and the cardiology fellow came by to get a sense of what happened – everything had to be documented. We explained in detail the change in Laura’s heart rhythm, her colour change and the events of earlier that day with her Troponin levels. Simon read back through her ECG report (which is printed automatically when an arythmia of any kind occurs – bradycardia included) and her code chart. He told us that it was less than 30 seconds from the time Laura’s heart rate dropped below 60 and when compressions began – that is an amazing feat and would have really helped in saving Laura’s brain function. The code lasted a total of 7 minutes from the beginning of compressions to when she regained consciousness. Suddenly I was so thankful that we had not been there when she had gone into cardiac arrest the first time – 7 minutes seemed like an eternity – the first time it was 90.
A.J and I walked down to the waiting room outside of the PCICU with Laura’s things. We knew the routine – it would be a while until anyone came to talk to us.
We spent time talking about what had happened and what might happen. Will she need ECMO – sure, maybe – we don’t care – ECMO saved her once, maybe it can do it again. Will she need a transplant? Maybe – actually, yes. How could we ever trust her heart again? We thought that this time it was fixed and this happened – there’s no way it could be trusted again.
Then the more difficult questions came – What if she’s not her anymore? What if her body can’t take any more? These are questions that you should not have to address for your baby but we did. If any of her organs are salvageable – we have to donate them. Something good has to come out of this.
We called our parents and siblings to give them the news. We kept it brief and felt awful for putting this on them but it was better than the alternative phone call – at least she was still with us.
After a little waiting, Dominic came out to talk to us. He explained that on the transport down to the PCICU Laura began looking very drowsy and was loosing colour. By the time they arrived in the unit, her heart beat was still registering but her pulse was barely palpable. Within another few minutes her colour faded to grey and he could not find a pulse – compressions began again.
They performed CPR for 30 minutes while the on-call surgeon placed her on ECMO.
This time, she had been cannulated (put on ECMO) through her neck – her internal jugular vein. The process was pretty well the same – the blood would be taken directly from the superior and inferior vena cavae and returning it to the right atrium as opposed to cannulation directly from her atria.
They were still working on her but Dominic said that we could come see her if we’d like – he was well aware that we were not shy around blood and other medical paraphernalia so he allowed us in a bit earlier than a newcomer to ECMO.
We walked into a familiar sight. It is not okay that none of what I saw stunned me. Laura had cannulae carrying blood from her right jugular vein to the ECMO circuit, she was hooked up to many lines, she was on a ventilator, she was covered in blood and she was grey. This time was different than last – through all of the machines, all I saw was my beautiful baby girl – alive.

We had a conversation with Dominic about next steps. He was frank in telling us that there were no guarantees – we wouldn’t know what damage had been done until we would be able to start waking her up a bit. She had suffered severe lung damage because during compressions, her mitral valve failed and the blood began flowing backwards into her lungs – they were trying to suction as much blood out as they could but they could only go so quickly. We spoke about transplant and he said they would have to discuss it with the team but he agreed with us – he did not feel that he could trust her heart again either.
We were given the code to the parent rooms and told to try to rest – it was well into the early morning hours and we needed to be well-rested for the many decisions that would be coming in the next hours and days.
Time to try to get some rest. I can’t believe this has happened again.
“The Lord himself goes before you and will be with you; he will never leave you nor forsake you. Do not be afraid; do not be discouraged.” Deuteronomy 31:8



2 thoughts on “Laura’s Story – Part 11 – the darkest hour – part II”